
I sit here on a Sunday night overwhelmed with the need to write this article. First of all because it’s important information that gets taken for granted and second of all because I am victim to what a brace can do. Ahhh…let’s go back a year. In February 2011 I broke my ankle while demonstrating push off during a running clinic I was hosting <—-I know that’s just sad isn’t it. I drove forward with my right leg and at the same time turned to answer a question. I rolled my ankle, only instead of a tolerable sprain I felt a nauseating crunch. With x-rays I found out I had an oblique fracture of my medial malleoli, a talar dome fracture, and at some point in my athletic history had avulsed my anterior talofibular ligament. I was put in a CAM walker for 6 weeks. I knew I hated boots after helping hundreds of patients rehab out of them, but I did not fully appreciate how much until I was in one. Now YES they are important, immobilization by the boot was preferable to fixation with a screw. I appreciate that. But what I want you to appreciate with this article is what the boot does that you don’t think about.
First, let’s talk about the height of the boot. It can cause at minimum a 1” leg length discrepancy depending on the height of the opposite leg shoe—and that’s when you are wearing shoes. That leg length discrepancy can wreak havoc on your sacroiliac joint. I have yet to have a patient come out of a boot that does not have a sacral torsion or inominate rotation and this is much more prevalent in females given increased ligamentous laxity. Patients assume their back pain is because of the boot—which it is—and that it will go away once the boot comes off—it does not. That rotation or torsion does not go away on it’s own. The body adapts to whatever position it is put in the most. That altered torque can cause a host of other problems. The pelvic obliquity causes a functional leg length discrepancy, and with that discrepancy comes compensation. The short leg can stay supinated trying to make up for the length loss. On the long leg the quadratus can shorten and the hip hikes up to try to accommodate for the length difference as well. This can cause increased torque in the spine and hip and lead to later disc issues or a higher risk for a labral tear in the hip.
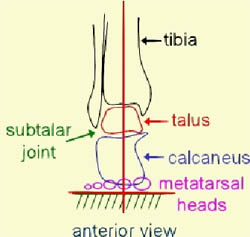
And what about the foot and ankle? Ahhh..that’s where the most damage is done—all in the good name of healing. So, we immobilize your foot/ankle to let it heal. That is the correct thing to do. However, what else happens because of that bracing. When we walk we want a great deal of subtalar mobility. When my foot hits the ground my calcaneus inverts, my midtarsal joint unlocks to absorb shock, and my tibia and femur internally rotate. All of this happens so that I can absorb the shock of the weight of my body meeting the ground and so I can turn on my powerful hip rotators in order to propel forward. As my body moves over my foot the opposite happens—my femur and tibia externally rotate, my calcaneus inverts, and my midtarsal joint locks up so that I have a rigid lever to push off of. It’s truly a great system—when it works. When we immobilize with a boot we stop this process from happening. And that’s good because we are protecting structures from force. However, once healed we need to restore this motion. Typically, after immobilization – both due to the boot itself and the swelling/soft tissue restriction of the injury—we lose subtalar joint motion. Which means we lose the ability to absorb shock and the ability to push off. This can put increased stress on joints and soft tissue. This can cause meniscus tears, labrum tears, plantar fasciitis, Achilles injuries, and soft tissue injuries such as chronic muscle strains.
Now let’s go back to my story. So I fractured a year ago, in boot for 6 weeks and went back to work. I exercise daily for my job. And what a difference a brace makes. I had no balance with any single leg exercise, could not squat symmetrically, had teeth rattling stiffness with all landing from jump—and that’s when I could jump 8 weeks later. My hip was sore, my knee was sore, my SI joint was torque. I strained my calf about 100 times showing people exercises in those first few weeks back as my body tried to find the path of least resistance to move.
That’s the key. On a base level our bodies are lazy. Subconsciously we find the easiest way to move. My body had chosen to externally rotate my right femur to try to gain motion with gait since I could not move through my subtalar joint. However, this didn’t go well. I have a high rigid arch, a plantar flexed first ray, and a tight hip. So instead, I strained my calf a half dozen times before I got it worked out. And it took help. This isn’t “go home and stretch and feel better,” I needed someone to make my subtalar joint and hip work together the right way. Looking back, I had probably not moved well in a long time. That old ATF tear happened when I was in high school. Back then, we iced, we braced, and we played. We were dumb. That mentality lead me to an ACL tear—however helped me pick a career so it’s a wash—grin.
So my point in all this…please send your patients to physical therapy after they have been in any sort of boot or post op shoe, give them firm guidelines on how long to wear any type of brace, and ask them about pain in other joints. A brace can be cumulative trauma. Poor motion causes inability to load and unload every joint in the chain resulting in increased stress, torque, muscle strain, and joint dysfunction.
– Alyssa Subbert, PT, CSCS, FAFS, FMR, CFCE, CEAS, NG360 GPS
Questions: Contact us at 987-6267 or alyssa@absoluteperformancetherapy.com.
