I coached volleyball and track for nearly ten years at both the junior high and high school levels. The beginning of the season always brought a new energy and a renewed passion for the sport. However, that was tempered by the seed of fear in the back of your mind about what if _____ got hurt, what would happen to your season. We all have those athletes, the super star scorer, the team leader, the one with blinding speed, the motivator. And, when those people get hurt it can devastate your season. So how do you prevent it? There are several pre-season cues that you can look for to tell you who has the greatest potential for injury and what type of injury that may occur. Let’s start at the bottom and work our way up.
Foot Position
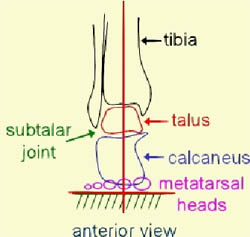
The position of a foot can predict a lot of injuries. If someone has a high rigid arch then they are more prone to ankle sprains. With a high arch the foot is carrying a majority of the weight on the lateral column (outside) and has greater ease of rolling. If you have a flat foot then you have less shock absorption available which can set you up for stress fractures, back pain, knee injuries, etc. If you have a good arch when sitting but it flattens when you stand then that is a sign that you have a weak glut medius. This is a glut muscle that supports all single leg activity. It is responsible for your ability to run, jump, cut, and land on one foot. Athletes with a strong glut med have less knee and ankle injuries, they are faster and have better reaction time on the run and off the jump. If this muscle is weak then the athlete has poor balance on one or two feet, puts more stress through their medial column (inside). This puts them at risk for ACL tears, ankle sprains, SI joint dysfunctions, patellar tendonitis, and plantar fasciitis, and stress fractures.
Knee Position
Genetics determines a lot about the position of your knee. If you have a strong valgus or knock knee-d posture then you are more at risk for ACL tears and typically have greater difficulty with jumping and cutting as a valgus knee position is less biomechanically efficient. If you add glut med weakness and a collapsing arch then your chances of injury are exponentially increased. Those with varus knee position or a bow legged appearance are at more risk for lateral ankle sprains, illiotibial band syndromes, hip bursitis, and have a difficult time with shock absorption with jumping. Knee position is directly effected by the strength of the gluts and the position of the foot.
Back Position

There are 3 load bearing curves in the spine: the neck curves in, upper back curves out and low back curves in again. These curves need to be in a good balance or you have an increased potential for injury as well as some pretty huge effect on performance. Chronic poor posture can effect these curves. If the upper back curve is excessive from chronic slumped positioning then the risk for shoulder impingements and neck pain is higher. Performance is effected as the athlete cannot fully extend upper back and therefore throwing velocity, vertical leap, and lung capacity can all be effected. Low back curve plays a large role in injury potential and performance as well. If the curve is too flat then low back pain can be due to poor shock absorption with running and jumping. Running speed and vertical leap can be effected as the hip has difficulty extending for end range push off with jump and stride length. If the curve is excessive then stability can be effected and increased stress can be placed on the base of the spine with all athletic activities. Performance can be effected as excessive curve leads to decreased hip flexion with running, poor reaction time off of the jump to cutting activities, weakness with full body contact, as well as poor control when attempting to stop motion. So, armed with all of this knowledge how do you prevent injuries. Take a look at your players posture. What are their backs doing? How do their knees line up with their feet? Do they have flat feet or high arched feet? Can they stand on one leg without losing their balance—if they can’t it’s pretty much a given that they have glut med weakness. When they squat do they assume a valgus knee position? If they do then they are at higher risk for knee and low back injury. Not only can you assess what injuries you may have but you may be able to understand the athlete’s limitations. If someone has a knock kneed posture it’s a lot harder to cut laterally and to jump quickly due to the biomechanical inefficiency of their leg. If you specifically train improved posture and mechanics with the activity they will get better. But yelling at them to get up higher or faster will never get results based on their underlying weakness and posture. If you have questions about your potential for injury or want ideas for warm ups for work outs to prevent injuries in any sport feel free to contact Alyssa Subbert, PT at Alyssa@absoluteperformancetherapy.com